When Mrs. Marty Mann announced the formation of the National Committee for Education on Alcoholism in 1944, she called upon local communities to establish a local alcoholism information center, a hospital-based detoxification unit, a clinic for the diagnosis and treatment of alcoholism, and rest centers for the long-term care of alcoholics. Since that time, and thanks to decades of advocacy efforts, communities across the country have made considerable progress in forging a continuum of care for individuals and families affected by alcohol and other drugs (AOD).
Early Intervention and harm reduction subsequently evolved as independent service components, and advocates are now calling for the formal inclusion of recovery support within this continuum of care. The danger with this latest addition is that recovery support will become an afterthought, a loosely attached appendage to addiction treatment or an isolated silo similar to how prevention, harm reduction, early intervention, and treatment now exist as separate fields/industries. As a field, we must instead fully infuse recovery as a catalytic concept and as a menu of support services within all of these arenas if there is to exist a true continuum of care. Here's why.
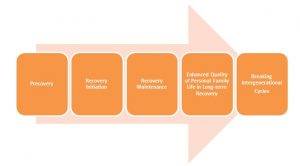
Prevention: No effective strategy for preventing the most severe, complex and chronic AOD problems can exist that fails to recognize the intergenerational transmission of addiction and related problems. The families and children of addicted and recovering people must be elevated as a priority population for prevention efforts. Effective prevention requires public modeling of responsible AOD decision-making and that such decisions can include the choice of abstinence for vulnerable populations and as a lifestyle preference. People in recovery can play an important part in breaking these intergenerational cycles and modeling responsible drug use decision-making and abstinence as a social value. People in recovery are at present the most untapped prevention resource.
Early Intervention: Unfortunately, the natural course of addiction can progress for many years before people seek help and initiate sustainable recovery. Shortening addiction careers and extending recovery careers would be a boon to affected individuals, families, and communities, but this would require sophisticated, assertive, and recovery-focused educational and outreach efforts. Part of such efforts would also require models of problem resolution and recovery support for people with lower levels of problem severity, complexity and duration. Achieving this would require increasing the visibility and accessibility of recovery within all major social institutions, including government, finance, business and industry, education, religion, health care, media, entertainment, criminal justice, and child welfare. People modeling multiple pathways and styles of recovery across diverse cultural contexts could play an important role in this process of education, early engagement, and recovery support.
Harm Reduction (HR): Dead people don't recover, and the current level of drug-related deaths is an American tragedy. People need different supports at different stages of their addiction and recovery careers. Those simple propositions marked the rationale for recovery advocates' support of and involvement in various HR activities. We need to meet people where they are but not leave them there without expanding their choices. We can both prevent harm and promote the capacity to flourish. We cannot offer support on people's journey from surviving to thriving if we turn our backs on them when they are at their worst. By integrating HR and recovery perspectives and practices, we can reduce the damage people carry with them into the recovery process. We can sustain life, enhance the quality of life, and expand choices for people at the precovery stage of their addiction and recovery careers. There will always exist tension between HR and recovery advocates, but we both serve our constituencies best in collaboration rather than in conflict and isolation.
Treatment: We, as a country and professional field, are routinely placing individuals with high problem severity, complexity, and chronicity in treatment modalities whose low intensity and short duration offer little realistic hope of sustainable recovery. When the resumption of drug use and its related consequences occur, we blame the individual rather than the flawed design of their treatment. Recovery advocates and their allies are working to shift addiction treatment from models of acute care to models of sustained recovery management (RM) nested within larger recovery oriented systems of care (ROSC). The calls for RM/ROSC represent a radical redesign of addiction treatment and the training of addiction professionals. This needed systems transformation process will only occur only through a sustained partnership between indigenous recovery communities and treatment policy makers and practitioners.
Recovery Support: Peer-based recovery support services are rapidly expanding in the U.S., in part as a Band-Aid on the acute care model of addiction treatment. The danger is that peer recovery support services will become the unpaid aftercare program for addiction treatment and the first services to be cast aside during in any future period of fiscal austerity. What is instead needed is the full integration of recovery support services across the continuum of care and across the stages of long-term personal and family recovery.
Infusion of recovery across the isolated silos that now represent the continuum of care will require recovery representatives within all of these arenas. Perhaps we can be the bridge people that help evolve these silos into a real integrated continuum of support for people experiencing AOD problems. What do you think?