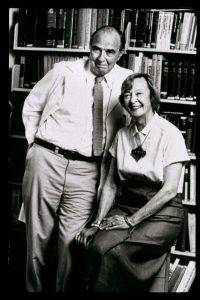
 Dr. Vincent Dole and Dr. Marie Nyswander Courtesy Dr. Vincent Dole
Dr. Vincent Dole and Dr. Marie Nyswander Courtesy Dr. Vincent Dole
Dr. Dole always regarded methadone as a legitimate medication to normalize aberrant metabolism and thus behavior in the chronic disease of opioid addiction. Dr. Dole was always at the service of patients and advocacy groups to help resolve issues of stigma and misdirected policies. --Herman Joseph and Joycelyn Sue Woods, 2006
In 1964, Dr. Vincent Dole and two colleagues, Dr. Marie Nyswander and Dr. Mary Jeanne Kreek, pioneered methadone maintenance in the treatment of heroin addiction. A half century later, their work stands as a pivotal milestone in the history of addiction treatment. Few subjects within the history of addiction treatment have elicited greater heat and less light than the rhetorical debates that long raged and continue today on methadone maintenance treatment (MMT). I have detailed earlier (see here) my transformation from a rabid critic of MMT (a role I acquired by osmosis during my early years in the field) to a supporter of MMT and other forms of medication-assisted treatment (MAT), even as I sought to elevate the quality of such treatments. The papers and speeches I made on MMT/MAT (see here, here, and here as examples) generated some of the harshest criticisms of my professional career.
As MMT passes the half century mark, I thought it appropriate to revisit some of the original MMT papers authored by Dr. Dole and co-authors. In rereading these early papers and Dr. Dole's later reflections on the evolution of MMT, I was struck anew by his passionate appeals for science-grounded addiction treatment and by his fierce loyalty to the needs of patients. I recalled that same passion when I interviewed him as part of my research for Slaying the Dragon.
All addiction professionals and recovery support specialists should be knowledgeable of the science and history of MMT. I have highlighted below some excerpts from the papers of Dr. Dole to provide some historical perspective on the evolution of methadone maintenance as practiced in the United States in Dr. Dole's own words. I hope to return later to highlight the thought and work of his collaborators, Dr. Nyswander and Dr. Kreek.
On His Initial Introduction to the Addictions Field.
I said what a shame it was that there was none of the scientific thought in the field of addiction that I had encountered in my other researches. It didn't have recognition as a scientific problem. (1989)
On Perception of Persons Addicted to Opiates.
. . . the traditional image of the narcotics addict (weak character, hedonistic, unreliable, depraved, dangerous) is totally false. . . .I had an exceptionally gifted teacher, Marie Nyswander, who taught me how to listen to patients rather than rush into their problems with pre-formed judgements. . . .the typical heroin addict is a gentle person, trapped in chemical slavery, pathetically grateful for understanding and effective treatment. In short, a sick person needing treatment. (1994a).
. . . it must not be too quickly assumed that these are weak individuals who would fail in society if relieved of the compulsion to obtain drugs. The potential strengths of addicts, like their faults, cannot be judged while the addicts are trapped in the orbit of drug abuse. (Dole & Nyswander, 1967)
Nature of Opioid Addiction / Rationale for MMT.
It is postulated that the high rate of relapse of addicts after detoxification from heroin is due to persistent derangement of the endogenous ligand-narcotic receptor system and that methadone in adequate daily dose compensates for this defectMethadone maintenance provides a safe and effective way to normalize the function of otherwise intractable narcotics addicts. (1988).
The most important principle to recognize is that addiction is a medical disease. And, as a medical disease, it's the responsibility of the medical profession. . . (1996).
It is important to distinguish the causes from the consequences of addiction . . . The rapid disappearance of theft and antisocial behavior in patients on the methadone maintenance program strongly supports the hypothesis that the crimes that they have previously committed as addicts were a consequence of drug hunger, not the expression of some more basic psychopathology. (Dole & Nyswander, 1967).
On Complexity of Opioid Addiction and MMT
I urged that physicians should see that the problem was one of rehabilitating people with a very complicated mixture of social problems on top of a specific medical problem. . . The strength of the early programs as designed by Marie Nyswander was in their sensitivity to human problems. The stupidity of thinking that just giving methadone will solve a complicated social problem seems to me beyond comprehension. . . (1989).
On Perception of MMT as Drug Substitution.
This medication given in fixed dose to tolerant subjects, does not make patients "high" or cause any other narcotic effects. On the contrary it eliminates the abnormal euphoric responses of addicts to narcotic drugs. (Dole, Nyswander, & Kreek, 1966).
What was not anticipated at the onset was the nearly universal reaction against substituting one drug for another, even when the second drug enabled the addict to function normally. . . . The analogous long term use of other medications such as insulin and digitalis in medical practice has not been considered relevant. (Dole & Nyswander, 1976).
On Functioning of MMT Patients.
Our patients are normally alert and functional; they live active lives, hold responsible jobs, succeed in school, care for families, have normal sexual activity and normal children, and have no greater incidence of psychopathology or general medical problems than their drug-free peers. (1988).
On Importance of Service Relationships within MMT.
Like teachers in a one-room school, we knew each patient personally. The ones in trouble were seen more often, the successful ones, less often; all were followed closely enough for us to know what they were doing. (1971)
I made a practice of spending two or three hours almost every day just sitting and talking with the addicts in a somewhat aimless way. I was just trying to get a sense of their way of thinking, their values, their experiences. They educated me about a world that was out of my reach, one that I had never been in and would never enter. (1989)
The most that any chemical agent can do for an addict is to relieve his compulsive drive for illicit narcotic. To give him hope and self-respect requires human warmth; to become a productive citizen he needs the effective support of persons who can help him find a job and protect him from discrimination. It is these human qualities that the treatment programs of the past five years have failed. (Dole & Nyswander, 1976).
. . . with addiction we're dealing with a disease in which human relationships are integral to rehabilitation. (1989)
On Early Fears about the Future of MMT.
The success of this treatment in rehabilitation of addicts will decline significantly if methadone programs cease to be medical institutions, and instead become instruments of another bureaucracy. (1971)
On Early MMT Expansion.
The difficulty was not that methadone expanded, or that it did so rapidly, but that it expanded faster than medical competence developed. . . . across the country people who had very little understanding of the pharmacology of methadone, and no comprehension of the wider array of medical and social problems presented by addicts, jumped into the field, feeling that all they had to do was hand out the drug. (1989).
. . . abstinence rather than rehabilitation was restored as the goal of treatment; doses were lowered to levels that were frequently inadequate; administrators became punitive and often contemptuous of the patients.(now calledclients. termination of maintenance was encouraged despite an 80% relapse rate. Underfunded, crowded, operating in poor quarters, harassed by teams of inspectors who criticized their deficiencies without providing money or political support for improvement, with a negative image fueled by disinformation in the media, the methadone clinics nevertheless survived, thanks to the dedication of their overworked staffs. (1999).
On Coerced Involvement in MMT.
Is it proper for a judge to force treatment on an addict by sentencing him to a maintenance program? Is it advisable for a physician to accept patients on these terms? I would say definitely no to both of these questions. . . . I would object to the imposition of methadone maintenance treatment just as strongly as I have objected in the past to its unavailability . . . (1971)
On Withholding or Reducing Methadone Dose for Rule Violations.
The results are generally poor, as might be expected from the fact that limiting or withholding medication that reduces drug hunger increases the need for illicit narcotics. (1988).
On Regulation of MMT.
Bureaucratic control of methadone programs has given us "slots", a rule book, and an army of inspectors, but relatively little rehabilitation.(Dole & Nyswander, 1976)
True patient-oriented treatment guidelines will emerge when the medical profession insists on applying the same standards of chemotherapy in addictions as it applies to chemotherapy in infectious disease, cancer, schizophrenia, depression, and endocrine disorders. (1992)
. . . the contempt with which many regulators and program administrators have treated their patients seems to be scandalous. (1996).
On Termination of MMT.
. . . methadone patients are not necessarily committed to a lifelong dependence on the medication. A significant fraction of the abstinent ex-addicts in New York today has previously been stabilized and socially rehabilitated in methadone programs. The key to this result is the realization that the most important objective in treatment of an addict is support of good health and normal function. This may or may not require continuation of maintenance. (1994).
The question of whether and when to discontinue methadone therapy can be answered in medical terms if the treatment is judged by the same standards as apply to other chronic diseases. (1973).
. . . the possibility of detoxification should be evaluated on an individual basis, taking into account the patient's own desires in the matter, his progress in rehabilitation, and the potential hazards of relapse. (Cushman & Dole, 1973).
On Predicting Positive Outcomes Following Termination of MMT.
Available data suggest that the longer a patient continues in a maintenance program that provides adequate doses (e.g., five years or more), the greater his or her probability of permanent abstinence after termination of treatment. Apparently, the neurochemical adaptations produced by thousands of heroin injections (with sudden impact on the nervous system and rapid elimination) are capable of gradual repair in some cases under the steady conditions of methadone maintenance. (1994).
On the Need for Post-MMT Recovery Checkups.
A good physician, experienced in treatment of chronic disease, will weigh these factors before attempting detoxification and will follow his patient for several years afterward, keeping the door open for return to maintenance if indicated. (1973).
On Patient Advocacy.
. . . I think methadone patient advocacy groups are going to grow in proportion to the numbers of people or programs who abuse their powers over methadone patients. (1996).
Future View of MMT.
I would say 30 years from now that current attitudes regarding methadone as substituting one drug for another and other negative outlooks on drug addicts in general will seem pretty archaic. What's happening today seems more like a carryover of medieval attitudes that affected much of the thinking toward mental illness in the last century. (1996).
Methadone is very valuable in controlling a specific kind of addiction, namely opioid addiction . . . But the emphasis should be on the fact that you're controlling the disease; you're not curing the disease. In time, and with full knowledge of all disturbances to in the neurohormonal systems in the brain, we may find ways to remedy and cure or restore a person tonormal.(1996)
On His Involvement with Alcoholics Anonymous.
. . . before accepting the position , I discussed my research with Executives of the fellowship and raised the question as to whether this appointment might involve a conflict of interest. . . . They insisted that they saw no problem. . . They were right. There never has been a problem in my association with AA, and my admiration for Bill Wilson and the dedicated AA members that I came to know increased over the years. (1991)
At the last trustee meeting that we both attended, he spoke to me of his deep concern for the alcoholics who are not reached by AA, and for those who enter and drop out and never return. . . . He suggested that in my future research I should look for an analogue of methadone, a medicine that would relieve the alcoholic's sometimes irresistible craving and enable him to continue his progress in AA toward social and emotional recovery, following the Twelve Steps. (1991).
References
Dole, V.P., & Nyswander, M.E. (1965). A medical treatment for diacetylmorphine (heroin) addiction. Journal of the American Medical Association, 193, 646-650.
Dole, V.P., Nyswander, M.E., & Kreek, M.J. (1966). Narcotic blockade. Archives of Internal Medicine, 118, 304-309.
Dole, V.P., & Nyswander, M.E. (1967). Heroin addiction. metabolic disease. Archives of Internal Medicine, 120, 19-24.
Dole, V. P. (1971). Methadone maintenance treatment for 25,000 addicts. Journal of the American Medical Association, 215, 1131-1134.
Dole, V.P. (1973). Detoxification of methadone patients and public policy. Journal of the American Medical Association, 226, 780-781.
Cushman, P., & Dole, V.P. (1973). Detoxification of rehabilitated methadone-maintained patients. Journal of the American Medical Association, 226(7), 747-752.
Dole, V.P., & Nyswander, M.E. (1976). Methadone maintenance treatment:A ten year perspective. Journal of the American Medical Association, 235, 2117-2119.
Dole, V. P. & Joseph, H. (1978). Long-term outcome of patients treated with methadone maintenance. Annals of the New York Academy of Science, 311, 173-180.
Dole, V.P. (1988). Implications of methadone maintenance for theories of addiction. The Albert Lasker Medical Awards. Journal of the American Medical Association, 260, 3025-3029.
Dole, V.P. (1989). Interview. In D. Courtwright, H. Joseph, and J. H. Des Jarlais, Addicts who survived (pp. 331-343). Knoxville, TN: The University of Tennessee Press.
Dole, V.P. (1992). Hazards of process regulation: The example of methadone maintenance. Journal of the American Medical Association, 267, 2234-2235.
Dole, V.P. (1994a). What we have learned from three decades of methadone maintenance treatment. Drug and Alcohol Review, 13, 3-4.
Dole, V.P. (1994b). Addiction as a public health problem. Alcoholism: Clinical and Experimental Research, 15(5), 749-752.
Dole, V.P. (1996). Interview with Dr. Vincent Dole, M.D.: Methadone: The next 30 years Addiction Treatment Forum, Winter, 1-6.
Dole, V.P. (1997). What is Methadone maintenance treatment.Journal of Maintenance in the Addictions, 1(1), 7-8.
Dole, V.P. (2002). Conversation with Vincent Dole. In G. Edwards (Ed.), Addiction: Evolution of a specialist field (pp. 3-10). Oxford: Blackwell Science Ltd. (Reprinted from Conversation with Vincent Dole, by Dole, V.P., 1994, Addiction, 89, 23-29).
Joseph, H., & Woods, J. S. (2006). In the service of patients: The legacy of Dr. Dole. Heroin Addiction and Related Clinical Problems, 8(4), 9-28.